By América Torres
Oscillometry is a non-invasive method to measure the mechanical properties of the respiratory system. This diagnostic tool enhances the valuable contributions of spirometry for the diagnosis, assessment, and monitoring of respiratory diseases such as asthma and COPD.
In this article, we will discuss the clinical advantages of oscillometry as a complementary method to spirometry. We will explore why it can provide healthcare professionals with a comprehensive overview that benefits patients with respiratory conditions.
Principles of Oscillometry
Principles of Oscillometry
Clinical Guidelines for asthma and COPD recommend the use of spirometry to quantify the degree of airflow obstruction. Spirometry involves performing an artificial forced expiratory maneuver from total lung capacity to residual volume. This means that spirometry induces volume-dependent closure of small airways.1
However, it's common for patients to find it difficult to perform the test properly, as the maneuver requires them to exhale forcefully down to residual volume. Therefore, it was necessary to find a simpler way to assess lung function in patients with asthma and COPD.
One of these methods is the Forced Oscillation Technique (FOT), which was originally described by Dubois et al.2 and later refined by Michaelson et al. by adding multiple frequencies.3 The FOT technique involves measuring the pressure/flow relationship (kPa/l.s) while forced oscillations of sound waves are imposed on normal tidal breathing to determine respiratory impedance.1
Oscillometry is based on FOT and is a noninvasive method for measuring the mechanical properties of the respiratory system. In the study "Clinical significance and applications of oscillometry,"4 it is mentioned that this technology measures the mechanical impedance of the respiratory system (Zrs), which represents the resistive and reactive forces that must be overcome to drive an oscillating flow signal into the respiratory system. According to the authors of that study,4 the forces arise in the respiratory system due to:
• The resistance of the airways and tissues to flow (Rrs).
• The elasticity (stiffness) of the lung parenchyma and chest wall in response to volume changes (encompassed in reactance, Xrs).
• The inertia of accelerating gas in the airways (Irs). Zrs has generally been reported at a single frequency or over the frequency range of 5-40 Hz as an average across the whole breathing cycle (i.e., both inspiration and expiration). It was also separately reported during inspiratory and expiratory phases in the mentioned study.4
In fact, the document mentions that oscillometry distinguishes adult asthmatics from healthy control individuals, as well as asthmatics with different degrees of airway obstruction. It was also useful in differentiating between groups of adults with asthma and those with COPD. Therefore, researchers suggest that oscillometry can be particularly helpful in diagnosing asthma in patients with preserved spirometry, as it is more sensitive to abnormal airway physiology.4
Oscillometry and Spirometry
Oscillometry and Spirometry
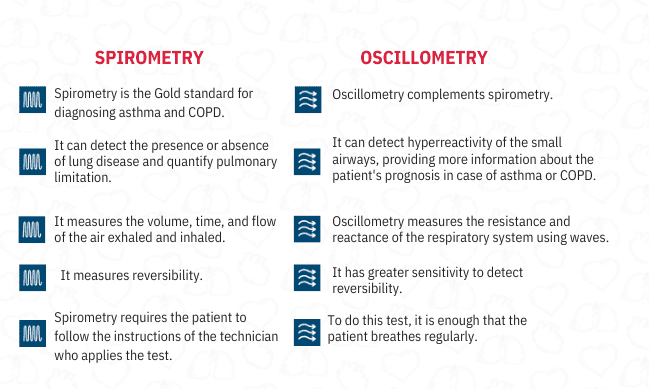
It is important to clarify that oscillometry and spirometry are not mutually exclusive tests, but rather complementary. Each offers unique insights that, when combined, enhance the information to provide healthcare professionals with a much broader view of the patient's lung condition. The following table summarizes the advantages of both:
Unlike spirometry, which mainly measures airflow rates, oscillometry focuses on the changes in impedance in the respiratory system in response to different frequencies of pressure oscillations.
So, what test should respiratory disease specialists use? While the measurement of absolute lung volumes and gas transfer provided by spirometry has been very useful for the clinical management and understanding of respiratory diseases, this test requires significant patient cooperation and willingness to perform maximal respiratory efforts. Oscillometry, on the other hand, is a non-invasive method of measuring the mechanical properties of the respiratory system, which can improve our understanding and management of lung diseases.
The mechanical properties of the lungs are disrupted in many disease states and exposures, contributing to significant respiratory symptoms such as dyspnea. Both clinical management and our understanding of respiratory diseases have benefited from widely available tests like spirometry and the measurement of absolute lung volumes and gas transfer. However, these measurements require significant cooperation from the patient and willingness to perform maximal respiratory efforts. Oscillometry is a noninvasive method for measuring the mechanical properties of the respiratory system, which can enhance our understanding and management of lung diseases.4
There are many cases in which the patient can benefit from oscillometry, for example4:
Response to bronchoprovocation. Several studies have shown that the response to bronchoprovocation (BDR) based on oscillometric parameters is better than one based on forced expiratory volume in 1 second (FEV1) in differentiating between asthmatic and healthy children. And this also applies to adult patients.
COPD. Oscillometry is useful for early detection of adverse effects of smoking before COPD is diagnosed.
Neuromuscular disease. In cases of patients with neuromuscular weakness, spirometry is not feasible as it requires muscular strength to generate the deep inspiration that this test demands. Therefore, the alternative is oscillometry.
Sleep apnea. Obstructive sleep apnea (OSA) is characterized by recurrent collapse and obstruction of the upper airways, resulting in nocturnal apnea and hypopnea. Since the increase in upper airway resistance is a distinctive feature of OSA, oscillometry is particularly suitable for detecting such airway obstruction.
Environmental and occupational exposure. It has been shown that firefighters and those exposed to asbestos have abnormalities in oscillometry parameters despite normal spirometric indices.
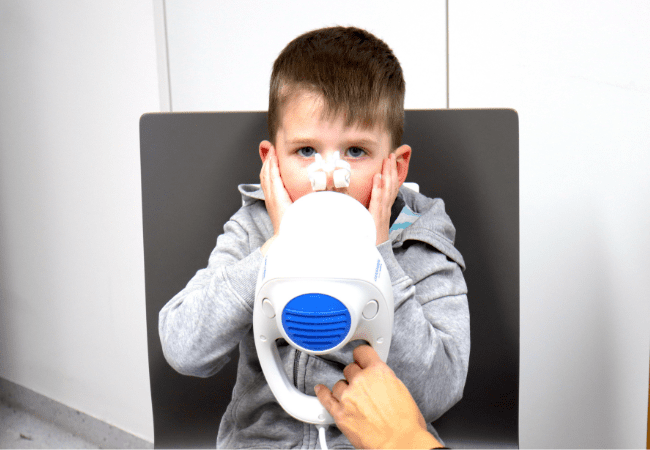
Children, elderly adults, impairment. Since oscillometry is a non-invasive technique that is well tolerated by patients of all ages – simply requiring them to breathe into the device's mouthpiece – it is particularly useful for this group of patients. It's also worth mentioning individuals who have difficulty following instructions due to mental or neurological reasons, physical impairments, or language barriers.
However, as we mentioned before. Oscillometry does not replace spirometry. It complements it. In fact, oscillometry could be a useful adjunct to spirometry in lung function tests of asthmatic children.5
Optimal detection
Optimal detection
Oscillometry offers a wide range of clinical advantages that, combined with the benefits of spirometry, allow lung health specialists to provide their patients with a comprehensive approach that encompasses early detection, timely diagnosis, proper management, and follow-up of response to treatment.
That is why SCHILLER-GANSHORN has expanded its line of pulmonary function equipment with the Airway Oscillometry System, tremoflo®. Now, respiratory health professionals have the ideal triad for lung health, including the PowerCube Body+plethysmography cabin, SpiroScoutultrasonic spirometer and tremoflo®. For more information about each device, click their names. If you´d like to see any of those devices in action, click the button below to request a demonstration.
REFERENCES
[1]I Say IOS You Say AOS: Comparative Bias in Respiratory Impedance Measurements Chris RuiWen Kuo et. al. https://link.springer.com/article/10.1007/s00408-019-00247-y
[2]Oscillation Mechanics of Lungs and Chest in Man. Dubois AB, Brody AW, Lewis DH, Burgess BF Jr (1956) J Appl Physiol. https://journals.physiology.org/doi/abs/10.1152/jappl.1956.8.6.587